The County operates three adult and two juvenile detention facilities in various geographic locations throughout the County. Each facility serves a unique population of individuals, with various underlying medical, psychological and social needs, at various stages of the criminal justice system. Today’s presentation will concentrate on the provision of mental health services across the spectrum of the criminal justice system, including pre-arrest, within the detention setting and upon release.
Pre-Arrest Efforts
A large number of individuals booked into County detention facilities have some type of mental health diagnosis. In recognition of that, and to proactively prevent those individuals from entering the criminal justice system due, in part, to their underlying illness, the County maintains initiatives to divert this population to appropriate treatment. One example of this is the newly established Mental Health Evaluation Teams (MHET).
In May 2015, the County, in partnership with the Contra Costa County Police Chiefs Association and the cities of Antioch, Concord and Richmond, established MHET teams composed of a police officer and a mental health clinician. MHET teams operate in police patrol vehicles and respond to requests from other patrol officers to provide welfare checks on residents following a psychiatric event, provide outreach to residents that may have a mental health diagnosis and support residents with household safety planning and resources.
In 2015, the MHET teams made 183 unique, client face-to-face contacts throughout the County.
Adult Detention Facilities
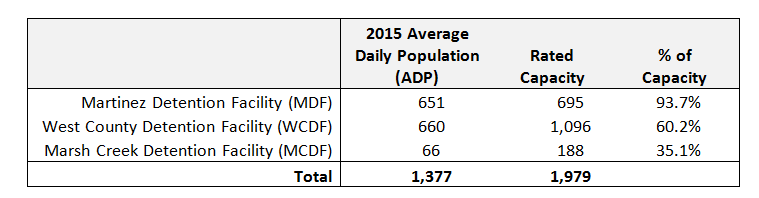
The County operates three adult detention facilities along with a custody alternative facility, which allows certain inmates to serve jail time outside of the detention setting. Below is a chart indicating the average inmate population vs. rated capacity at each facility:
The above ADP information is critical to understanding the needs of an in-custody population; however, it is equally important to illustrate the volume of individuals making contact with the County jail system. In 2015, the Sheriff’s Office received 26,296 bookings, or 72 per day. This is up 9.4% from 2014.
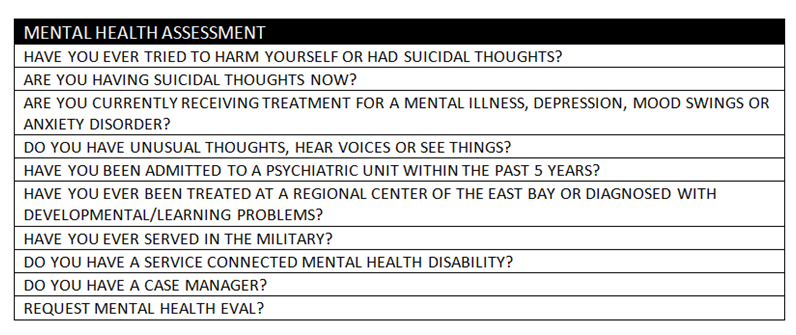
All adult bookings are completed at the MDF, which includes a mental health screening. This screening is completed by nursing staff from the Health Services Department (HSD) operating within the facility. Below is the ten-step Mental Health Assessment used during booking screenings:
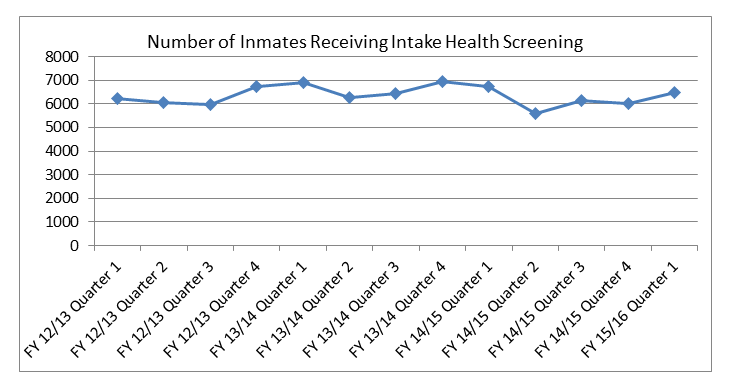
Over the past several years, HSD staff has averaged between 6,000-7,000 mental health screenings, at booking, per quarter. Should an inmate being booked answer “yes” to any of the above screening questions, a comprehensive mental health assessment is performed. The mental health assessment includes a psycho-social and mental status evaluation. Below is a chart illustrating this trend since fiscal year 2012/13:
Following booking, an intake health assessment and a mental health screening, the Sheriff’s Office, in consultation with Mental Health staff in the facility, may assign a special classification to the inmate should there be evidence of an existing mental health issue. This is similar to many other populations with special classifications housed within the detention facility, including those with affiliation with a gang or in other protective custody.
Typically, special populations, including those required to take medication for mental health needs, are exclusively housed at the MDF. Below is a listing of certain special classifications and the amount of inmates assigned to each as of January 2016:
Current Special Classification Inmate Populations – January 2016
- Mental Health - 343
- Protective Custody - 220
- Gang Affiliation - 200 (those are only the known members)
- Penal Code 187 (Murder) - 142
- Administrative Segregation – 94
Once in the facility, mental health services are limited to crisis intervention. Group therapy sessions are not offered at MDF primarily due to the high inmate census and restrictions in the physical plant. Specifically, there are no group therapy rooms or “no-contact” visiting rooms for individual counseling sessions. Ultimately, the MDF was not designed with the provision of comprehensive mental health treatment in mind.
More severe cases include inmates that have been deemed “incompetent to stand trial” and must be returned to competency prior to prosecution of the case. Most felony incompetent to stand trial cases in this category are the responsibility of the Department of State Hospitals (DSH). Currently, DSH has a significant backlog of bed space available for this population. For example, Napa State Hospital has a 6-8 month waiting list to be enrolled into a program.
For misdemeanor defendants deemed incompetent to stand trial, County Forensic Mental Health Services (FMHS), within the Behavioral Health Division, provides outpatient restoration of competency treatment. Since beginning in June 2011, FMHS has received 120 court orders for restoration of competency treatment. Of those, 16 have been transferred to DSH for additional treatment. Most FMHS referrals are seen in the community.
The Public Defender’s Office advises that approximately 300 clients have been deemed incompetent to stand trial since 2012. The shortage of appropriate State beds has put continued stress on the local detention facilities and created a backlog of cases within the local criminal justice system.
Other alternatives to the State Hospital system have been available, including those counties with facilities able to care for this population. Contra Costa County has maintained a contract with Santa Clara County for one such bed. This has allowed the County to transfer inmates throughout the year to that program, including five in 2014 and twelve in 2015. In late 2015, Santa Clara County announced that they will no longer be offering that service.
Juvenile Detention
The County operates two juvenile detention facilities, including the Juvenile Hall and the Orin Allen Youth Rehabilitation Facility (OAYRF). The County’s juvenile mental health infrastructure is robust and includes a wraparound component once juveniles are released from the facility.
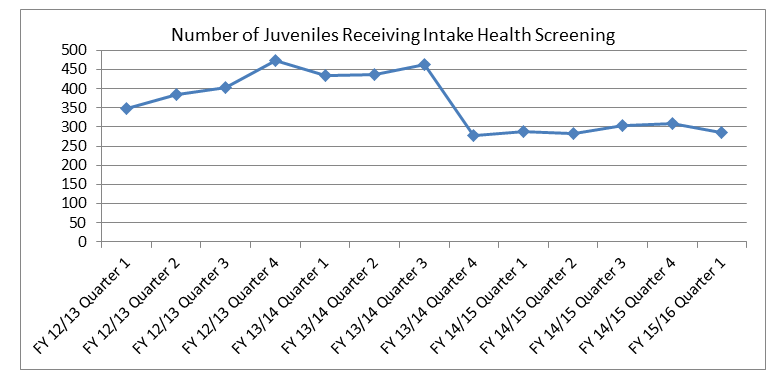
Juvenile bookings average 90-100 per month at the Juvenile Hall. Similar to adult bookings, each juvenile is administered the brief mental health screening discussed previously by HSD nursing staff. It is estimated that approximately 60% of juveniles booked have some kind of mental health diagnosis. Below is a chart illustrating the number of juveniles receiving an intake health screening at the Juvenile Hall:
Once booked into the facility, juveniles may be assigned to a treatment unit. The Juvenile Hall is composed of eight units, two of which provide comprehensive treatment services. The Youthful Offender Treatment Program (YOTP) serves up to thirty boys within the facility while the Girls in Motion (GIM) program serves up to fifteen girls.
Juvenile Hall provides behavioral health services seven days per week (clinicians are on site from 9:00 am to 7:30 pm). Staff includes one full-time program manager, two full-time licensed clinicians, one 0.8 FTE licensed clinician, and three 0.5 FTE clinician trainees. Additionally, psychiatric services are available on Tuesday and Thursday (psychiatrist is on site from 9:00 am-2:00 pm). Health Services nursing staff is on site daily from 7:00 am to 10:45 pm with physician services available on site Monday through Friday and on call after hours.
Transitioning from In-Custody to Outpatient Care
Adult Populations
For adults, Behavioral Health collaborates with Adult Felony Probation to serve specific populations, including both AB 109 clients released from state prison and general supervision clients released from county jail.
In March 2012, the Forensic Mental Health Services (FMHS) unit within Behavioral Health Division began accepting referrals and providing services to clients. The team is comprised of 3 clinicians, 2 peer specialists, 1 Registered Nurse and a 0.2 FTE prescriber. From March 2012 through December 2015, FMHS has made a total of 864 unique, face-to-face contacts with individuals on adult felony probation.
Referrals are identified by probation status:
- AB 109 – 500 referred, 303 contacted;
- General Supervision- 800 referred, 561 contacted
Clinicians are co-located at the three, regional adult probation offices. The referral process involves Deputy Probation Officers who schedule clients for screenings with the clinicians. The intake process involves clinicians screening clients for voluntary services within the Physical and Behavioral Health Systems of Care. Services include screening and assessment, health care navigation, benefit support, psychiatric case management and group facilitation at Probation, including Seeking Safety Trauma groups and Wellness Recovery Action Plan (WRAP) groups.
Juvenile Populations
Juveniles being released from detention facilities have several services in place for continuity of care upon release. Specifically, Behavioral Health maintains clinicians at regional Probation offices, similar to the adult populations, which juvenile Deputy Probation Officers can refer clients to for services. In addition, Probation provides a cascade of transition services for youth returning to the community, including:
- The Youth Justice Initiative, funded by the Byrne Justice Assistance Grant (JAG) last year, is in the early stages of implementation. Among other things, this initiative aims to ensure that juveniles receive appropriate care upon release by providing additional assistance to both the youth and families.
- The Mentally Ill Offender Crime Reduction (MIOCR) Grant is funding a Functional Family Therapy (FFT) program targeting juveniles released from the YOTP or GIM programs identified above. Probation hopes to expand this program more completely to the OAYRF in the future; however, a small amount of referrals have been made from OAYRF.
- Multisystemic Therapy (MST) is a family based, in home program. The goal of MST is to assist and enable caregivers to appropriately set (and manage) expectations, impose structure, and enforce consequences. Services are intensive, consisting of multiple (in home) sessions per week.
- Multidimensional Family Therapy (MDFT) is another in home, family based therapy targeting co-occurring substance abuse issues that negatively impact family and community functioning.
Challenges and Considerations
The County places significant resources in the provision of mental health services at all phases of the criminal justice system. It is important to continue reviewing challenges that arise during the provision of those services and evaluate considerations for service delivery.
Challenges and Opportunities for Improvement
- Lack of capacity in community for critical, outpatient substance abuse programs
- Accessibility to outpatient mental health appointments upon release from detention
- Willingness of client to continue treatment post-release
- Family unwilling or unable to assist youth in continuation of treatment post-release
- Limitations of the physical plant at the MDF to facilitate comprehensive mental health treatment
- Continued backlog at State Hospitals for treatment of inmates deemed incompetent to stand trial
- Continue to seek funding for construction of mental health beds within County detention facilities
- Continue support of pre-arrest mental health efforts, including MHET, sobering centers and other diversion programs
- Build capacity within the community for needed behavioral health programs, including substance abuse programs
- Advocate for additional funding of State Hospitals for return to competency treatment
This report is informational only.
Speakers: Ralph Hoffman; Teresa Pasquini; Lauren Rettagliata; Joseph Partansky